It’s familiar cocktail party trivia by now: you have more bacterial cells in your body than human cells. Gross and fascinating, it’s a perfect conversation bomb, a welcome diversion from work chat or the cultural importance of Taylor Swift. What, actually, is a human body, one is left to wonder? Are these microorganisms simply fellow travellers – given that they are separate from the cells carrying our DNA? Or are they, more fundamentally, us?
Prepare to peel off another layer of that philosophical onion. Not only do we carry around a veritable Serengeti of bacteria and protozoa and fungi, we also each have a personalised set of viruses that interact with them and with our own cells.
You might think about it like this: if bacteria and other single-celled organisms are the lions and the wildebeest, romping over our carefully moisturised hides, stalking their way through nearly all our organs, viruses are the diseases that infect them, keeping populations in check or in some cases simply hitching a ride. It is an imperfect metaphor – particularly given the fact that some of these viruses also infect our own cells – but it gives you a general idea.
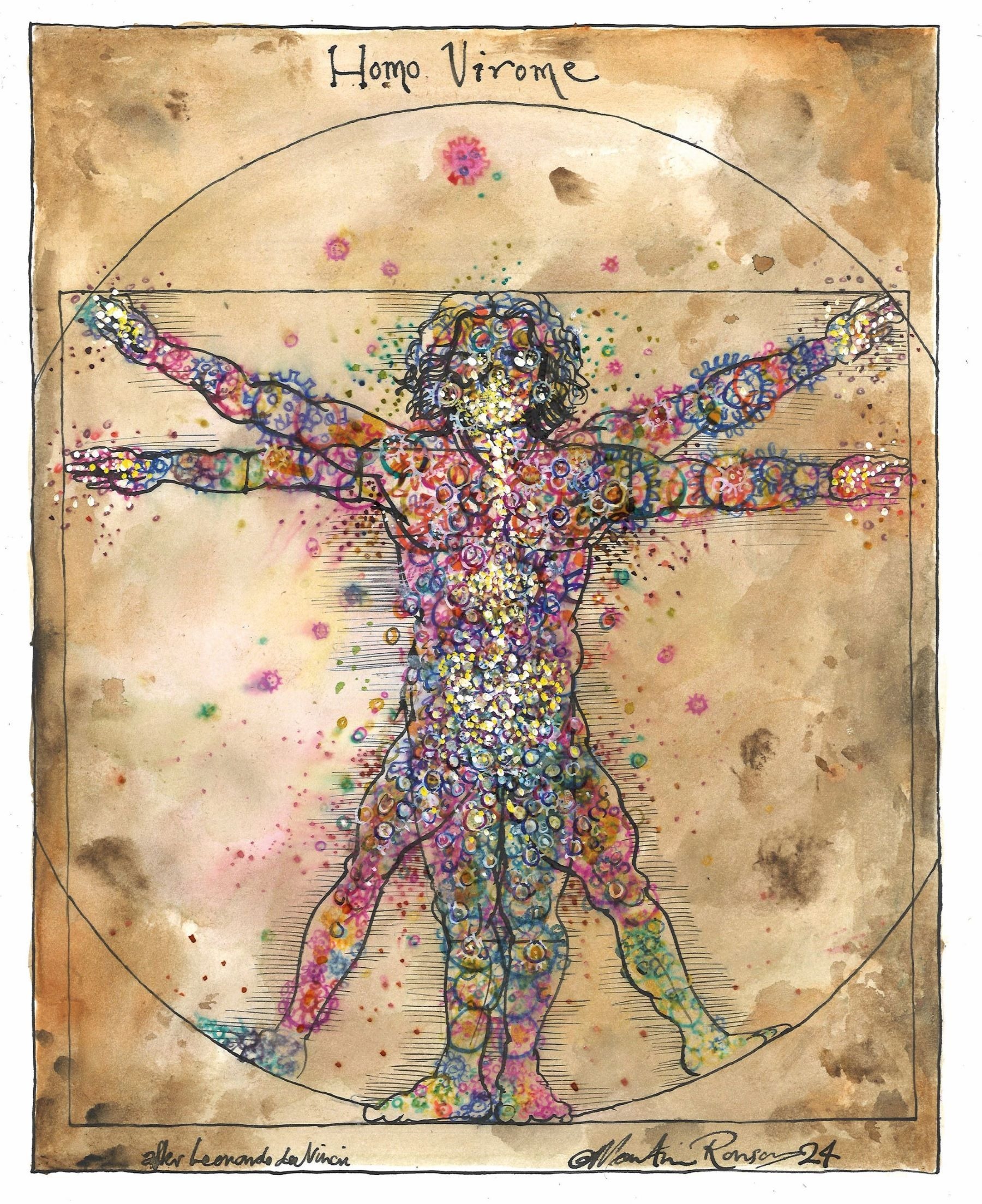
This is the virome: a suite of mysterious entities that appears to be equally as crucial to the cascading processes that keep us alive as the microbial component we are just
beginning to understand. The perfect metaphor to describe the virome remains elusive because we know so little about it. In fact, depending on who you ask, we don’t even know if viruses are truly alive. Perhaps in this alien, microscopic version of the Serengeti, viruses are something closer to robot hyenas. Like robots, they operate mindlessly, with one goal in mind – in this case, replicating their code. And like hyenas, they mercilessly gang up on their prey, which may itself be a predator.
Of course, we are all too familiar with the nearly 300 pathogenic (disease-causing) viruses that give us, for example, the common cold or Covid-19. But not many people know about the tens of thousands of other species that inhabit our bodies without causing apparent harm, at least most of the time. Some viruses lie in wait, only becoming pathogenic under certain circumstances. Others never cause disease at all. A large proportion are bacteriophages – phages for short – that infect the bacteria that colonise us as well.
Like the explorers of yore who catalogued the species inhabiting distant lands, virologists are now attempting to discern how exactly they affect our health – and our evolution. “We’ve been co-evolving with viruses for so long,” says Eric Delwart, a virologist at the University of California, San Francisco. “Probably since the very beginning of life itself.”
Forensic potential
Imagine it’s the near future. You are a jewel thief and are executing your latest heist. You’ve hacked the CCTV, secured a stolen vehicle for your escape and zipped yourself into a latex suit to contain the DNA your body is sure to shed. But, in a moment of carelessness, a sliver of skin grazes the safe. It’s not enough to leave behind an appreciable amount of DNA (you’ve depilated your entire body, of course) but you nonetheless give the detectives something to work with: a tiny smear containing millions of bacteria and viruses. And that cocktail of invisible creatures is just as unique as a fingerprint. How, exactly, the prosecutor later asks, did your little crew of hitchhikers end up on the handle of the safe at Tiffany’s?
Viruses may soon be a useful secondary option when DNA is not available at a crime scene. While far from being a commonly used investigative tool, the early results of research are promising. There are going to be more viruses in any given sample than there are bacterial or human cells. And there will also be more variety, allowing for the establishment of a unique fingerprint with greater certitude.
The forensic value of the virome relies in part on the stability of its composition. One study that looked at the viromes of 42 people over a six-month period found them to be relatively constant. The researchers collected samples from both hands and from the scalp. “In every single person, there was some amount of variability,” says co-author Michael Adamowicz, director of the forensic science program at the University of Nebraska-Lincoln. But the array of species was still distinctive. “The most important question is: do you put enough of those viruses on the object to be able to tell you from somebody else?” And the second: “How long does it last?”
Still, the authors point out that identification of more viral families is required to improve the accuracy of these tests. “An awful lot of our skin virome is not defined,” Adamowicz says. “The species of viruses are not characterised. Nobody has any idea what they are.”
One of the main distinguishing factors was the presence of viral particles associated with domestic animals. “That’s not surprising,” Adamowicz says. “Some of our participants worked with animals, and therefore they had unique viral particles that the rest of us didn’t have. We found that there was a strong ability to identify people who owned cats.”
While virome analysis may be used in future for scenarios like that of the jewellery theft, it will likely be even more useful in cases where humans contact each other. Viral contamination could provide evidence in such challenging cases as sexual assaults in which human DNA is difficult to differentiate – for example, when penetration has been digital. Because the traces of human DNA will be faint and mixed with the victim’s in these cases, the virome could be a clearer means of linking the attack to the perpetrator.
The human polyomavirus 2 (also called the John Cunningham virus) is present in up to 90 per cent of the population and is found in the gut, the kidneys and even the brain. Forensic scientists in Japan are already using the different strains of the virus to identify human remains. Analysing the geographically distinct and stable genotypes helps narrow down the origin of the cadaver in question.
Health benefits
But we still don’t know what the virome is exactly, or how it’s developed. We do know that all of us emerge from the womb virtually sterile, although some viruses are likely transmitted during passage through the birth canal (babies born by Caesarean section have lower viral diversity). After that, we quickly pick up our microbiomes – including our viromes – through our diets, from the people we come into contact with, and from the environment.
Mother’s milk appears to be particularly important. Viruses begin showing up in infant faeces mere days after they are born. They seem to ride in, on or inside bacteria that are transmitted through breastfeeding. Indeed, viruses that have the potential to become pathogenic are less numerous in infants who are breastfed, suggesting that the beneficial viruses transmitted by the mother have a mediating effect.
Geography appears to play a role as well – John Cunningham virus is not the only one to exhibit distinct geographical signatures. Studies of people living in different regions of the same country have demonstrated that the environment in which people live, even if separated by a few hundred miles, can result in appreciable differences in virome composition.
And though viromes appear to be relatively stable over long periods, discernible differences have been observed even during short stretches of contact. People who have lived together for only a few days were shown to have picked up components of each other’s viromes.
These hitchhiking entities grow in number and diversity as we age. They have even shaped how we operate as organisms. Perhaps most famously, the gene that codes for the protein required for the formation of the placenta was derived from a virus that inserted itself into the genetic code of a mammalian ancestor. Such viruses are known as retroviruses – they insert a DNA copy of their RNA genome, altering the host genome from that point forward. Mammals, it can thus be inferred, would not have evolved were it not for the mindless intervention of a virus at some point in our prehistory. Your birth and mine were the long tail of an ancient genetic accident.
This is hardly an anomaly, though the additional effects of viral entry into the genome are poorly understood. Some 8 per cent of the human genome is thought to be viral in origin. “These retroviruses have become us or we’ve become them,” Delwart suggests. “We couldn’t live without them. We wouldn’t be alive.”
Even some frighteningly recognisable viruses can play a beneficial role. Hepatitis G, which infects around 16 per cent of the population without apparent effect, appears to slow the progress of HIV, for example. Other types of hepatitis are highly pathogenic.
The same is true of herpes viruses, which are strongly associated with a range of different cancers, but also appear to protect against such diseases as bubonic plague (in mice, at least).
“Once you have them, you never really get rid of them. They just go dormant. And whenever you are stressing out or you’re starving, they will pop back out of the reservoirs and could make you sick,” Delwart warns.
From hero to villain
Other viruses that lurk in the system suddenly become harmful given the right conditions. The Epstein-Barr virus, for example, is present in 90 per cent of people but is linked to severe disease in only a small number. In inflammatory bowel disease (IBD) patients, a particular suite of viruses correlates to the disorder, while a different complement of viruses is found in healthy patients.
Viruses even regulate immune system responses – which, when they misfire, are responsible for a whole host of pathologies. Of course, when these responses are operating as they should, they keep us healthy. Imbalances in the virome increased susceptibility to Covid-19 infection. Strangely, low levels of pepper mild mottle virus, which is obtained through eating peppers and likely does not actually permanently integrate into the human virome, correlated to a greater chance of Covid-related illness.
The factors that tip the balance in such situations are not well understood. What changes a seemingly benign virus into an entity that threatens our lives or disables us? In the gut, dietary factors play a role. Studies indicate that certain compounds in food lead to an increase in phage populations and thus inhibit the growth of the bacteria they infect. The opposite must be true as well. “You may have a great microbiome and one day you’ll be eating something that contains a phage that is going to wipe out some of those good bacteria,” Delwart says.
In all likelihood, the correlations between viral populations and disease are reflective of highly complex, delicate relationships between those viruses, the microbes they infect, the environment the person inhabits, what they ingest, their inherent genetic makeup and a host of other factors that have yet to be identified. Correlation is one thing, causality another.
You’ve completed your sentence for the jewel heist: 10 long years in jail. Finally, tasting freedom, you feel a cramping in your gut. Prison food didn’t agree with you, but this is something more concerning. You may have some form of IBD – you see blood in the toilet. But all is not lost. The same technology that put you behind bars may be able to help your guts.
The therapeutic application of viruses dates back more than a century. Felix d’Hérelle first began administering phage therapy in 1919, curing people of dysentery caused by Shigella bacteria. Phages were at the centre of the 1925 Sinclair Lewis novel Arrowsmith, in which the protagonist uses them to cure an outbreak of bubonic plague. Leveraging viruses native to the human body has received increased attention in recent years as a potential pathway to curing disease without the use of harsh, chemical-based therapies.
Studies in mice have shown increased inflammation when certain intestinal viruses are depleted, while the reintroduction of viral compounds alleviated the disease. Phages that target E. coli have shown promise in treating Crohn’s disease – a form of IBD. And in patients suffering from Clostridium difficile, a bacterium that can cause disease of the digestive system, faecal transplants have proven effective, even when the bacterial components were filtered from the faeces, leaving only viral particles. The viruses contained in a stranger’s turd could have life-saving potential.
So, this horde of strange things marching up and down our spines, skittering over our skin and waging war in our intestines may make or break us. They may even be the key to understanding life itself. In the meantime, know that each time you open a door, or swipe your credit card or use the toilet, you leave a phalanx of your own personal viral army behind.
This article is from New Humanist’s summer 2024 issue. Subscribe now.

